Tweet
Objective: To determine the level of evidence based practice (EBP) among nurses in hospitals, and to analyse its association with the nursing practice environment (NPE), the professional experience, and the EBP training.
Method: Cross-sectional study. Data were collected from nurses in the Regional University Hospital of Málaga (Spain) between February and May 2019. The inclusion criteria were: (1) Spanish-speaking nurses who work in the Regional University Hospital of Málaga; and (2) those who had signed an informed consent. For the evaluation of the EBP level, the Health Sciences-Evidence Based Practice Questionnaire (HS-EBP) was used. NPE was evaluated with the Practice Environment Scale-Nursing Work Index (PES-NWI).
Results: 99 nurses participated in the study. The mean total score of HS-EBP was 380.39 (SD 67.39). EBP was positively correlated with NPE in hospitals and with EBP training. A negative relationship between EBP and professional experience was found.
Conclusions: The EBP among nurses in hospitals is positively related to the NPE in hospitals and to EBP training and negatively related with professional experience. NPE is a critical factor that can facilitate EBP among nurses.
Keywords:
Evidence-Based Practice;
Nurses;
Health Sciences;
Nursing, Practical.
INTRODUCTION
Evidence based practice (EBP) is defined as ‘the integration of the best research evidence with clinical expertise, patient values and the use of current best evidence in making decisions about the care of individual patient (18).
Despite nursing general awareness of the importance of EBP, there is a gap between nursing research and practice (21). In this context, EBP is not still common among nurses, the clinical decisions being rarely based on the best available evidence. (16;18). As a result, quality of care provided by nurse practitioners can be suboptimal, and it can have a negative impact on patient safety and on the the quality of services (8;14).
EBP among nurses can be influenced by several factors, such as professional knowledge and experience, nursing education, self-confidence, and the nursing practice environment (NPE) (1;6;8;19). In this regard, NPE is defined as ‘organisational characteristics of a work setting that facilitate or constrain professional nursing practice’, and it play an important role in the development of EBP among nurses. (1;15).
There is little available evidence on the measurement of EBP among nurses and its relationship to NPE, professional experience, and EBP training in Spanish culture. Given this concern, we decided to carry out a cross-sectional study to determine the level of EBP among nurses in hospitals, and to analyse its association with the NPE in hospitals, professional experience, and EBP training. Therefore, the aims of this study were to: (1) determine the level of EBP among nurses in hospitals, (2) explore the association between EBP and NPE in hospitals, (3) explore the association between EBP and professional experience, and (4) explore the association between EBP and EBP training.
METHODS
Design
This research was carried out using a cross-sectional and correlational design as part of a larger study in which we measured the impact of the implementation of best practice guidelines in beliefs, attitudes and behavior related to evidence based practice and nurse's work environment. This article concentrates only on the descriptive data of the level of EBP among nurses in hospitals, and it explores the association of the level of EBP with the NPE in hospitals, professional experience, and EBP training.
Participants
Participants were recruited at the Regional University Hospital of Málaga (Spain), as part of a larger study. The inclusion criteria were: (1) Spanish-speaking nurses who work in the Regional University Hospital of Málaga; and (2) those who had signed an informed consent. The exclusion criteria used was: nurses that at the time of the
data collection are not laborly active.
Data collection
The data were collected between February and May 2019.
Sociodemographic data on participants were obtained (age, sex, marital status...)
Participants who met the inclusion criteria were selected. Nurses were contacted to inquire about their availability to participate in the study. Nurses who wanted to participate were informed about the procedure and the protection of personal data, and after that, they received the documents to complete. Questionnaires were self-administered.
Questionnaires
Health Sciences-Evidence Based Practice Questionnaire (HS-EBP). The HS-EBP is a valid and reliable instrument to assess the EBP in Spanish population (9). This instrument has showed satisfactory psychometric properties in terms of content validity, internal consistency, structural validity and convergent validity (9).
It consists of 60 items that can be rated on a 10-point Likert scale according to the degree of agreement (greater score, greater degree of agreement). These items cover five domains: “Beliefs and attitudes” (12 items); “Results from scientific research” (14 items); “Development of professional practice” (10 items); “Evaluation of results” (12 items) and “Barriers / Facilitators” (12 items) (9). A higher score indicates a better level of EBP.
Practice Environment Scale-Nursing Work Index (PES-NWI). The PES-NWI is a valid and reliable instrument to assess the NPE in Spanish population (4;12). This instrument has demonstrated the best coverage of psychometric properties in terms of content validity, reliability, structural validity, concurrent and discriminant validity (4;12;20). The PES-NWI comprises 31 items that can be rated on a 4-point Likert scale and it is structured in 5 factors: participation of the nurse in the centre’s affairs; nursing principle of care quality; provision of capacity, leadership and support to nurses by nursing managers; staff size and adequacy of human resources; and relationships between physicians and nurses (15). A higher score indicates a better practice environment perceived by nurses (20).
Ethical considerations
The Provincial Ethics Committee of Málaga has approved this study. The standards of good clinical practice and the ethical principles established for research in human beings were maintained. Clinical data were separated from personal identification data to assured confidentiality. Before participation in the study, nurses received information about the content and the study aim and gave their written consent.
Data analysis
A descriptive analysis was carried out to obtain the demographic and clinical data. We determined the distribution and normality of the sample by performing a one-sample Kolmogorov–Smirnov (KS) test (significance p >0.05). To explore the association between EBP and NPE, the Pearson correlation coefficient was used. The Pearson´s correlation coefficient used the criteria of poor (r<0.49), fair (r=0.50-0.74) and strong (r>0.75). The value of p<0.05 was taken as statistically significant. The statistical programs SPSS version 20.0 was used to carry out the data analysis.
RESULTS
Characteristics of sample
The KS test [Asymp. Sig. (2-tailed) = 0.9] indicated that the sample was normally distributed.
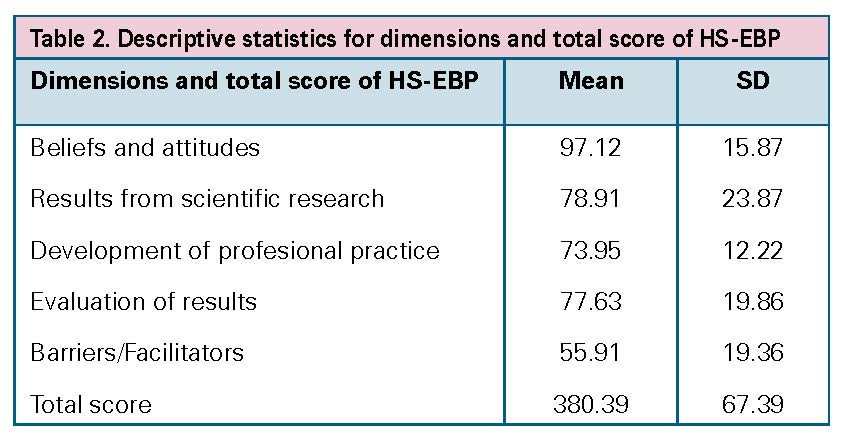
One hundred eighty nurses were identified. One hundred eight surveys were returned and 9 cases were eliminated due to the high percentage of unanswered items. Finally, 99 nurses participated in the study (Figure 1). The majority of nurses were females with a mean age of 42.3 (SD 8.4) (Table 1). Of the 99 participants, 15.1% had a Master, and 2% had a PhD. Moreover, 24% had learned about EBP. The mean total score of HS-EBP was 380.39 (SD 67.39) (Table 2). The missing values did not exceed 2%.
Figure 1. Participant flow
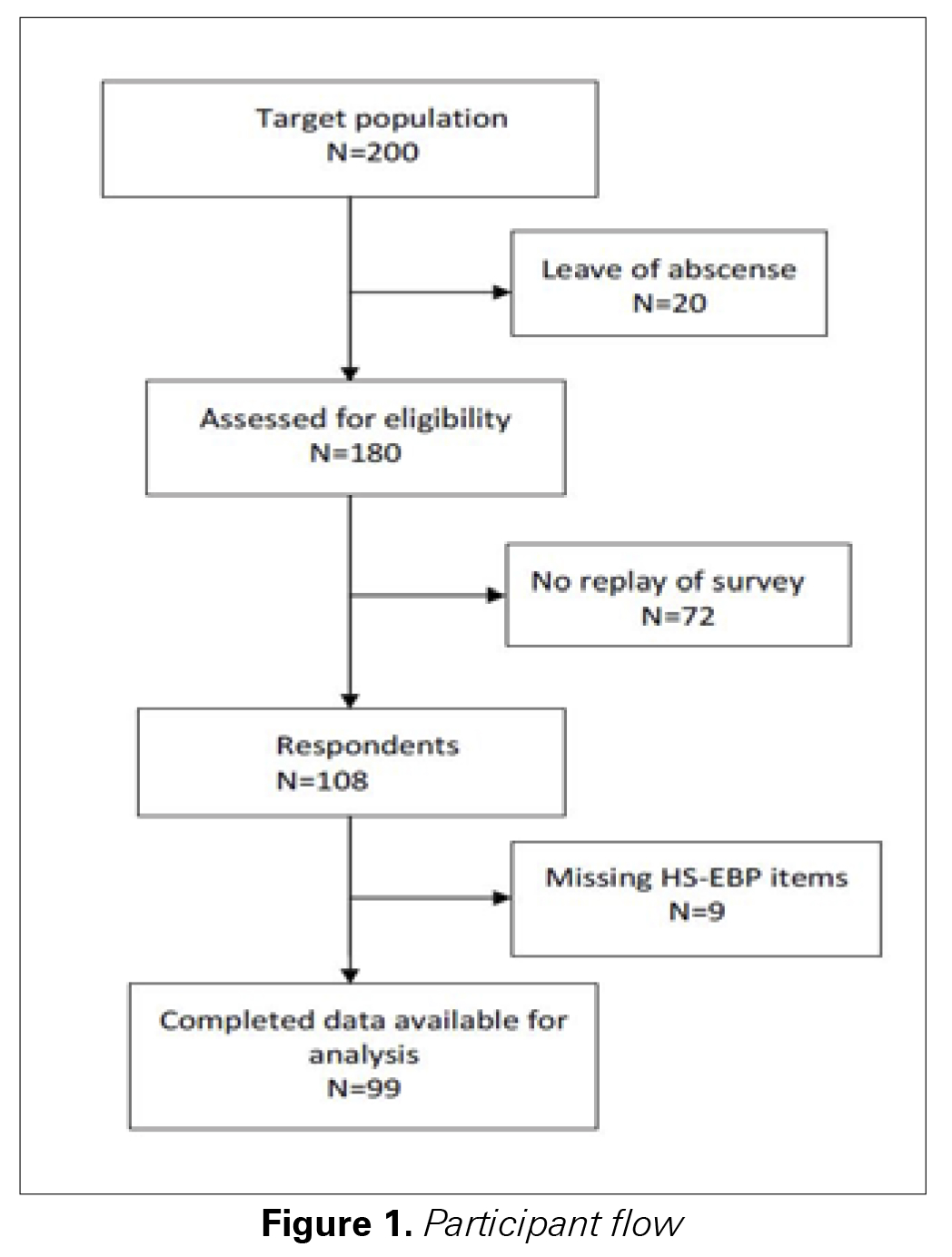
Table 1. Characteristics of the sample (N=99)
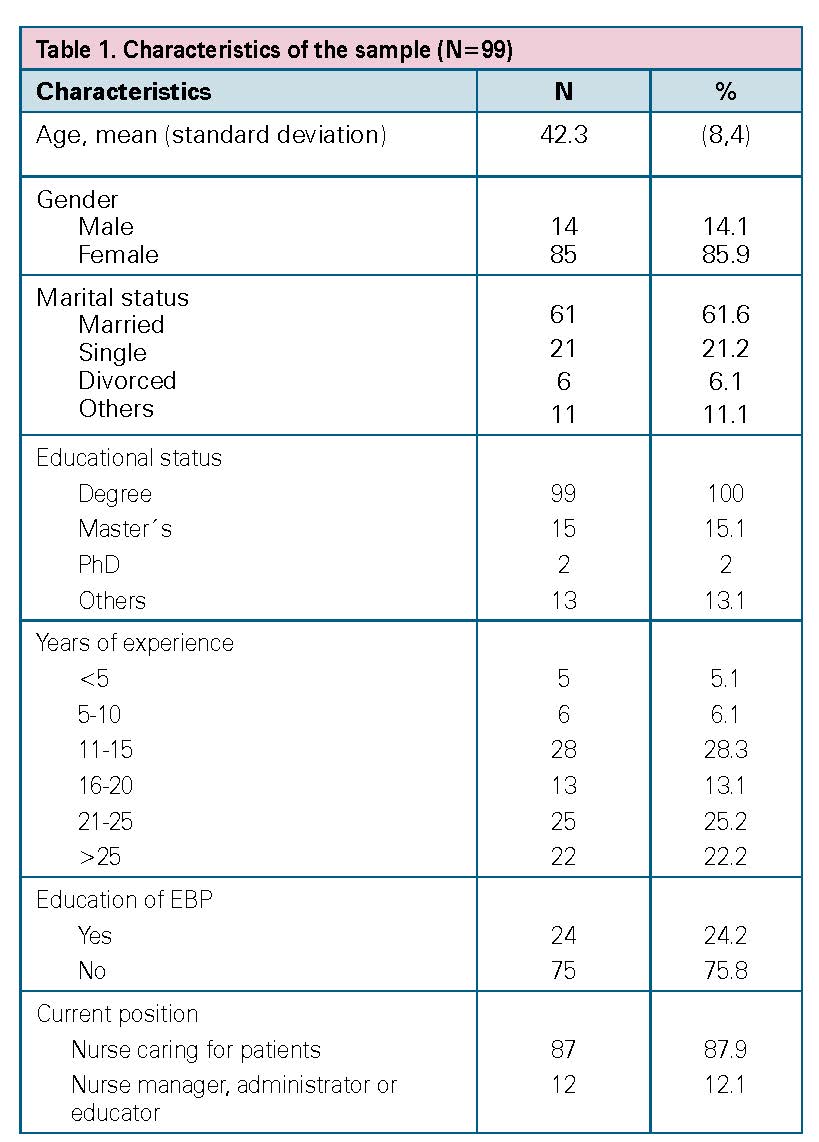
Table 2. Descriptive statistics for dimensions and total score of HS-EBP
Association between EBP and the NPE in hospitals
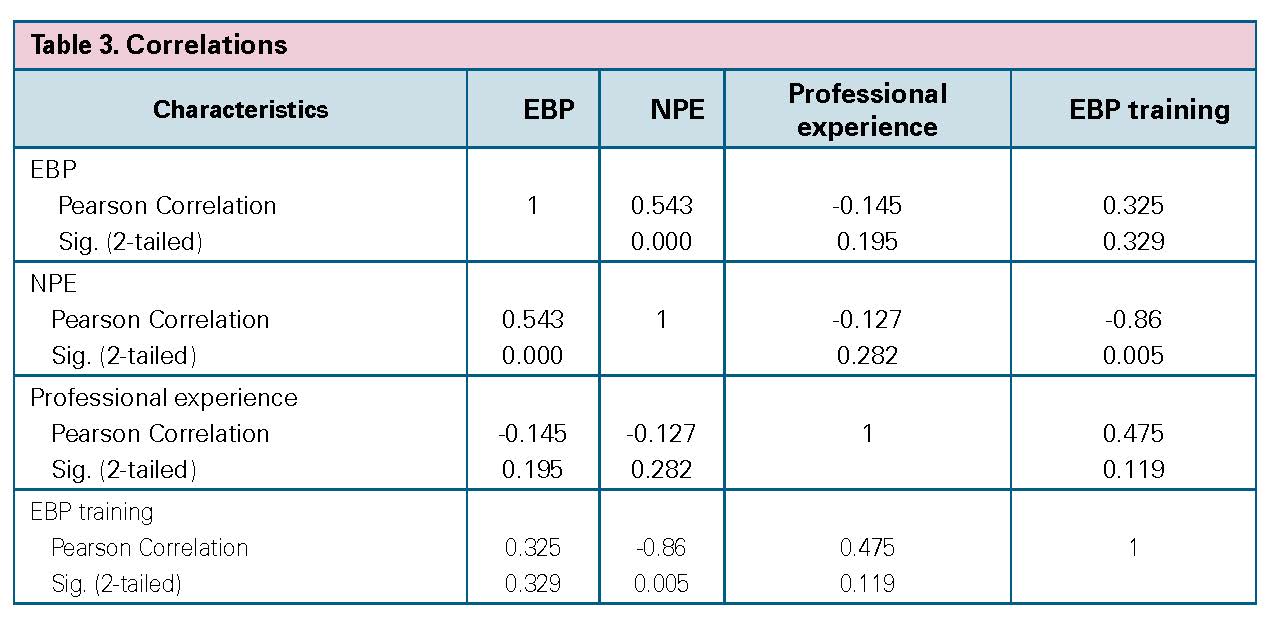
The association between EBP and the NPE in hospitals was explored (Table 3). The results indicated that there was a positive and statistically significant relationship between these two variables (r = 0.54, p < 0.001), and therefore the EBP was higher when the NPE in hospitals was high.
Association between EBP and the professional experience
The association between EBP and the professional experience was also explored. The results indicated that there was a negative relationship between EBP and professional experience (r = -0.14). This relationship wasn´t statistically significant (p = 0.19).
Association between EBP and the EBP training
The relationship between EBP and EBP training was also evaluated. The results showed that there was a positive relationship between EBP and EBP training (r = 0.32), and therefore the EBP was higher when nurses have received EBP training. This relationship wasn´t statistically significant (p = 0.32).
Table 3. Correlations
DISCUSSION
The EBP approach to nursing practice play a fundamental role in providing the highest quality and most cost-efficient patient care possible.
This is the first study performed in Spain in which the level of EBP among nurses in hospitals and its relationship with the NPE in hospitals, professional experience, and EBP training is analysed.
Factors, such as NPE, professional experience, and the EBP knowledge, play an important role in the implementation of EBP among nurses. In this regard, the results of this study showed adequate values of EBP among nurses in hospitals (380.39 SD 67.39). These values were positively related to the NPE in hospitals (r = 0.54, p < 0.001), and therefore the EBP was higher when the NPE in hospitals was high. Along this line, the results of others studies indicated that NPE is a critical factor in facilitating or inhibiting EBP (1).
However, a negative relationship between EBP and professional experience (r = -0.14) was found. These results are comparable to those obtained in other studies (13).
Concerning the relationship between EBP and EBP training, a poor and positive relationship was found (r = 0.32), and therefore the EBP was higher when the EBP training was high.
The American Association of Colleges of Nursing (AACN) identify the dimensions that describe the characteristics of the environment of practice that best support the professional practice of nursing that works to its fullest potential: a clinical care philosophy emphasizing quality, safety, interdisciplinary collaboration, continuity of care and professional responsibility, the promotion of nursing leadership at the executive level and the maintenance of clinical progress based on education, and certification and advanced preparation among others (5). In this context, the work environments perceived by nurses have an impact in the results in the health of patients, the perception of the quality of care provided, as well as in health outcomes (2;3;7).
EBP among nurses requires the creation of an environment that allow to increase the use of evidence in practice.
However, the majority of hospitals and nurses are not implementing the available evidence and guidelines for providing the best care in their practices (11). This suggests an even greater imperative to implement the best practice guidelines into practice environments.
Further studies in which we measure the impact of the implementation of best practice guidelines in beliefs, attitudes and behavior related to evidence based practice and nurse's work environment are needed.
Limitations of the study
There are some limitations in this study. This is a cross-sectional study that has been conducted in one centre. Thus, our results may not be generalizable because the cohort does not represent the broader population of nurses in hospital. Further longitudinal studies in which we measure the impact of the implementation of best practice guidelines are needed.
1. Adib-Hajbaghery, M. (2007). Factors facilitating and inhibiting evidence-based nursing in Iran. Journal of Advanced Nursing, 58(6), 566–575. https://doi.org/10.1111/j.1365-2648.2007.04253.x
2. Aiken, L. H., Sermeus, W., Heede, K. V. den, Sloane, D. M., Busse, R., McKee, M., … Kutney-Lee, A. (2012). Patient safety, satisfaction, and quality of hospital care: Cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ, 344, e1717. https://doi.org/10.1136/bmj.e1717
3. Aiken, L. H., Sloane, D. M., Clarke, S., Poghosyan, L., Cho, E., You, L., … Aungsuroch, Y. (2011). Importance of work environments on hospital outcomes in nine countries. International Journal for Quality in Health Care: Journal of the International Society for Quality in Health Care, 23(4), 357–364. https://doi.org/10.1093/intqhc/mzr022
4. Alzate, L. C. C., Bayer, G. L. A., & Squires, A. (2014). Validation of a Spanish version of the practice environment scale of the nursing work index in the Colombian context. Hispanic Health Care International: The Official Journal of the National Association of Hispanic Nurses, 12(1), 34–42. https://doi.org/10.1891/1540-4153.12.1.34
5. American Association of Colleges of Nursing. (2002). Hallmarks of the professional nursing practice environment. Journal of Professional Nursing: Official Journal of the American Association of Colleges of Nursing, 18(5), 295–304.
6. Carlson, C. L., & Plonczynski, D. J. (2008). Has the BARRIERS Scale changed nursing practice? An integrative review. Journal of Advanced Nursing, 63(4), 322–333. https://doi.org/10.1111/j.1365-2648.2008.04705.x
7. Cho, E., Chin, D. L., Kim, S., & Hong, O. (2016). The Relationships of Nurse Staffing Level and Work Environment With Patient Adverse Events. Journal of Nursing Scholarship: An Official Publication of Sigma Theta Tau International Honor Society of Nursing, 48(1), 74–82. https://doi.org/10.1111/jnu.12183
8. Dalheim, A., Harthug, S., Nilsen, R. M., & Nortvedt, M. W. (2012). Factors influencing the development of evidence-based practice among nurses: a self-report survey. BMC Health Services Research, 12, 367. https://doi.org/10.1186/1472-6963-12-367
9. Fernández-Domínguez, J. C., Sesé-Abad, A., Morales-Asencio, J. M., Sastre-Fullana, P., Pol-Castañeda, S., & de Pedro-Gómez, J. E. (2016). Content validity of a health science evidence-based practice questionnaire (HS-EBP) with a web-based modified Delphi approach. International Journal for Quality in Health Care: Journal of the International Society for Quality in Health Care, 28(6), 764–773. https://doi.org/10.1093/intqhc/mzw106
10. Fernández-Domínguez, J. C., de Pedro-Gómez, J. E., Morales-Asencio, J. M., Bennasar-Veny, M., Sastre-Fullana, P., & Sesé-Abad, A. (2017). Health Sciences-Evidence Based Practice questionnaire (HS-EBP) for measuring transprofessional evidence-based practice: Creation, development and psychometric validation. PLoS ONE, 12(5). https://doi.org/10.1371/journal.pone.0177172
11. Fischer, F., Lange, K., Klose, K., Greiner, W., & Kraemer, A. (2016). Barriers and Strategies in Guideline Implementation—A Scoping Review. Healthcare, 4(3). https://doi.org/10.3390/healthcare4030036
12. Fuentelsaz-Gallego, C., Moreno-Casbas, M. T., & González-María, E. (2013). Validation of the Spanish version of the questionnaire Practice Environment Scale of the Nursing Work Index. International Journal of Nursing Studies, 50(2), 274–280. https://doi.org/10.1016/j.ijnurstu.2012.08.001
13. González-Torrente, S., Pericas-Beltrán, J., Bennasar-Veny, M., Adrover-Barceló, R., Morales-Asencio, J. M., & De Pedro-Gómez, J. (2012). Perception of evidence-based practice and the professional environment of Primary Health Care nurses in the Spanish context: A cross-sectional study. BMC Health Services Research, 12(1), 227. https://doi.org/10.1186/1472-6963-12-227
14. Kristensen, N., Nymann, C., & Konradsen, H. (2016). Implementing research results in clinical practice- the experiences of healthcare professionals. BMC Health Services Research, 16(1), 48. https://doi.org/10.1186/s12913-016-1292-y
15. Lake, E. T. (2002). Development of the practice environment scale of the Nursing Work Index. Research in Nursing & Health, 25(3), 176–188. https://doi.org/10.1002/nur.10032
16. Melnyk, B. M., Fineout-Overholt, E., Feinstein, N. F., Sadler, L. S., & Green-Hernandez, C. (2008). Nurse practitioner educators’ perceived knowledge, beliefs, and teaching strategies regarding evidence-based practice: Implications for accelerating the integration of evidence-based practice into graduate programs. Journal of Professional Nursing: Official Journal of the American Association of Colleges of Nursing, 24(1), 7–13. https://doi.org/10.1016/j.profnurs.2007.06.023
17. Sackett, D. L., Rosenberg, W. M., Gray, J. A., Haynes, R. B., & Richardson, W. S. (1996). Evidence based medicine: what it is and what it isn’t. BMJ (Clinical Research Ed.), 312(7023), 71–72. https://doi.org/10.1136/bmj.312.7023.71
18. Saunders, H., & Vehviläinen-Julkunen, K. (2016). The state of readiness for evidence-based practice among nurses: An integrative review. International Journal of Nursing Studies, 56, 128–140. https://doi.org/10.1016/j.ijnurstu.2015.10.018
19. Solomons, N. M., & Spross, J. A. (2011). Evidence-based practice barriers and facilitators from a continuous quality improvement perspective: An integrative review. Journal of Nursing Management, 19(1), 109–120. https://doi.org/10.1111/j.1365-2834.2010.01144.x
20. Swiger, P. A., Patrician, P. A., Miltner, R. S. S., Raju, D., Breckenridge-Sproat, S., & Loan, L. A. (2017). The Practice Environment Scale of the Nursing Work Index: An updated review and recommendations for use. International Journal of Nursing Studies, 74, 76–84. https://doi.org/10.1016/j.ijnurstu.2017.06.003
21. Thorsteinsson, H. S., & Sveinsdóttir, H. (2014). Readiness for and predictors of evidence-based practice of acute-care nurses: A cross-sectional postal survey. Scandinavian Journal of Caring Sciences, 28(3), 572–581. https://doi.org/10.1111/scs.12083
22. Wallen, G. R., Mitchell, S. A., Melnyk, B., Fineout-Overholt, E., Miller-Davis, C., Yates, J., & Hastings, C. (2010). Implementing evidence-based practice: Effectiveness of a structured multifaceted mentorship programme. Journal of Advanced Nursing, 66(12), 2761–2771. https://doi.org/10.1111/j.1365-2648.2010.05442.x